Anemia occurs when there aren’t enough healthy red blood cells to carry oxygen to your body’s organs. As a result, it’s common to feel cold and symptoms of tiredness or weakness. There are many different types of anemia, but the most common type is iron-deficiency anemia. You can begin to ease symptoms of this type of anemia by adding iron to your diet.
What is anemia?
Anemia happens when you don’t have enough red blood cells or your red blood cells don’t work as they should. Your red blood cells carry oxygen throughout your body. Oxygen powers your cells and gives you energy. Without healthy red blood cells that do their job, your body doesn’t get the energy it needs to function. While some types of anemia are short-term and mild, others can last for a lifetime. Left untreated, anemia may be life-threatening.
How does anemia affect my body?
When someone develops anemia, they’re said to be anemic, meaning they have symptoms of anemia, like being very tired or feeling cold all of the time. Anemia affects different people in different ways:
- Newborns: Some infants are born with low red blood cell counts. Most newborns don’t need medical treatment for anemia, but some with severe anemia may need blood transfusions.
- Infants: Infants may get less iron than they need when they start eating solid food. That’s because the iron in solid food isn’t absorbed as easily as iron in breast milk or formula. Infants with anemia may appear lethargic.
- Children: Children do a lot of growing between birth and age 2. Children going through growth spurts need more iron. Children with anemia may develop related problems such as delayed development of motor skills and issues with learning.
- Women who are pregnant: Women who are pregnant may develop iron-deficiency anemia, which may increase the chance of complications such as premature birth or giving birth to babies with low birth weight.
- Women and people designated female at birth (DFAB): Women and people DFAB who have heavy periods (menstrual bleeding) or conditions like uterine fibroids may lose blood and develop anemia.
- People age 65 and older: People over 65 are more likely to have iron-poor diets and certain chronic diseases that increase their risk of developing anemia. If they develop anemia, they may have heart conditions or weakness that makes it hard for them to get around. They may have confusion or depression.
- People with chronic conditions: Some chronic conditions like autoimmune diseases or cancer may increase the risk of anemia. This is anemia of chronic disease.
How common is this condition?
Anemia is very common, affecting an estimated one-third of the global population and an estimated 3 million people in the United States.
What are the types of anemia?
There are many anemia types, each causing red blood cell levels to drop.
Nutritional anemias
- Pernicious anemia: Pernicious anemia, one of the causes of vitamin B12 deficiency, is an autoimmune condition that prevents your body from absorbing vitamin B12.
- Iron-deficiency anemia: As its name implies, iron-deficiency anemia happens when your body doesn’t have enough iron to make hemoglobin. Hemoglobin is the substance in your red blood cells that enables them to carry oxygen throughout your body.
- Megaloblastic anemia: Megaloblastic anemia is a type of vitamin deficiency anemia that happens when you don’t get enough vitamin B12 and/or vitamin B9 (folate).
Inherited anemias
- Sickle cell anemia: Sickle cell anemia changes your red blood cells’ shape, turning round flexible discs into stiff and sticky sickle cells that block blood flow.
- Fanconi anemia: Fanconi anemia is a rare blood disorder. Anemia is one sign of Fanconi anemia.
- Diamond-Blackfan anemia: This inherited disorder keeps your bone marrow from making enough red blood cells.
Anemias caused by abnormal red blood cells
- Hemolytic anemia: In this anemia, your red blood cells break down or die faster than usual.
- Aplastic anemia: This anemia happens when stem cells in your bone marrow don’t make enough red blood cells.
- Autoimmune hemolytic anemia: In autoimmune hemolytic anemia, your immune system attacks your red blood cells.
- Sideroblastic anemia: In sideroblastic anemia, you don’t have enough red blood cells and you have too much iron in your system.
- Macrocytic anemia: This anemia happens when your bone marrow makes unusually large red blood cells.
- Microcytic anemia: This anemia happens when your red blood cells don’t have enough hemoglobin so they’re smaller than usual.
- Normocytic anemia: In this type of anemia, you have fewer red blood cells than usual, and those red blood cells don’t have the normal amount of hemoglobin.
What are the symptoms of anemia?
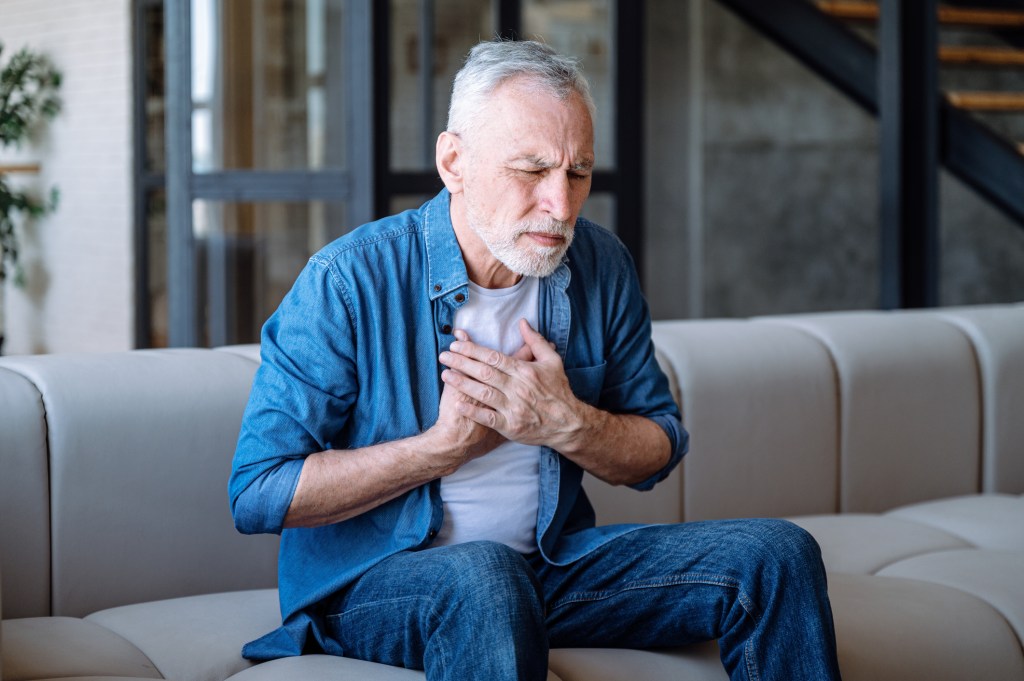
Fatigue — feeling too tired to manage your activities — is the most noticeable anemia symptom. Other symptoms may include:
- Shortness of breath (dyspnea): This is the feeling you can’t catch your breath or take a deep breath.
- Dizziness: This is feeling lightheaded or unsteady on your feet.
- Fast or irregular heartbeat (arrhythmia): This is when your heart feels like it’s racing or skipping beats.
- Pounding or “whooshing” sound in your ear (pulsatile tinnitus): This is a swooshing sound in one of your ears that may come and go.
- Headache: Iron-deficiency anemia and anemias caused by low hemoglobin may cause headaches.
- Pale or yellow skin: Your skin color may be paler than usual.
- Chest pain: This may feel like something is pressing on or squeezing your chest.
What is the main cause of anemia?
People may be born with certain types of anemia or develop anemia because they have certain chronic diseases. But poor diet causes iron-deficiency anemia, which is the most common form of anemia.
How do healthcare providers diagnose anemia?
Your healthcare provider will ask questions about your symptoms. As anemia happens when you don’t have enough healthy red blood cells, they’ll do blood tests to check on your red blood cells:
- Complete blood count (CBC): Healthcare providers use this test to check on all of your blood cells, with a focus on your red blood cells. They count your red blood cells and evaluate your red blood cells’ size and shape. Healthcare providers may use this test to check on your vitamin B12 or B9 levels.
- Peripheral blood smear: Healthcare providers examine your red blood cells under a microscope.
How do healthcare providers treat anemia?
First, your healthcare provider will determine if you have anemia caused by a poor diet or a more serious health problem. They may refer you to a hematologist, a healthcare provider who specializes in blood disorders. Here are some examples of common anemia treatments:
- Healthcare providers may recommend changing your diet or taking supplements if you have iron-deficiency anemia or pernicious anemia.
- If you have anemia because you have a chronic disease, your provider will treat the underlying condition. They may prescribe medication to boost red blood cell production.
Providers may use medications like immunosuppressants or treatments like blood transfusions to treat anemias that happen when you have abnormal red blood cells, like aplastic anemia or hemolytic anemia.
Can I prevent developing anemia?
You can’t prevent some kinds of anemia, such as sickle cell anemia, hemolytic anemia or aplastic anemia. People with chronic diseases who may develop anemia should watch for anemia symptoms. And you can prevent nutritional anemias by eating a healthy diet.
What can I expect if I have this condition?
Your prognosis or expected outcome depends on why you have anemia, the type of anemia you have and whether you have a severe form of it. Most of the time, healthcare providers can treat anemia by helping you manage your diet or with medications. But there are times when you may be living with anemia for the rest of your life.
What happens if anemia isn’t treated?
People who have undiagnosed or untreated anemia may have life-threatening organ failure. Children who have severe anemia may have developmental delays. People in their 80s may develop heart conditions, including angina, arrhythmias and myocardial infarction.
How do I take care of myself?
While some types of anemia are short-term and mild, others can last for a lifetime. There are several ways to help manage anemia, including:
- Following a healthy diet: Poor diet is the primary reason why people develop anemia. Ask your healthcare provider about iron-rich foods and other foods you should eat.
- Drinking enough water to stay hydrated.
- Getting regular exercise: Check with your healthcare provider about ways to exercise safely.
- Avoiding exposure to certain chemicals: Exposure to certain metals may cause hemolytic anemia.
- Washing your hands often to avoid infection: You may also want to ask your healthcare provider about vaccines that defend against common infections.
- Taking good care of your teeth and going to the dentist regularly: Iron-deficiency anemia may cause dental problems.
- Tracking your symptoms and letting your healthcare provider know about any changes.
When should I see my healthcare provider?
If you have anemia, you should check with your provider if your symptoms get worse despite treatment or if you notice changes in your body that may be new symptoms of anemia.
When should I go to the emergency room?
Anemia may increase your risk of a heart attack. Call 911 if you have the following symptoms:
- Trouble breathing.
- Nausea.
- Sweating.
- Chest pain
What questions should I ask my healthcare provider?
Anemia may affect your body in many ways. It may happen for many different reasons. If you’re concerned about developing anemia or you have anemia, here are some questions you may want to ask your healthcare provider:
- What kind of anemia do I have?
- What caused it?
- What treatments do you recommend?
- When will I start to feel better?
- How long will I need treatment?
- Can you cure my anemia?
A note from QBan Health Care Services
Anemia happens when you don’t have enough red blood cells or your red blood cells aren’t working as well as they could. Some people are born with forms of anemia, but most people who have anemia develop the condition over time. That’s why it’s important to keep track of changes in your body. For example, we all have days when we feel worn out. But if you’re feeling very tired for several days despite getting rest, consider talking to your healthcare provider. Most of the time, anemia is a short-term issue easily treated by changing your diet or taking supplements. Untreated, anemia may cause serious medical issues.